No content results match your keyword.
Content
You have successfully logged out.
Not registered yet?
No content results match your keyword.
Content
No product results match your keyword.
Products
Peripheral IV Catheters
Blood spillage and exposure to blood not only displays a risk but also interrupts the tight workflow of hospital staff. B. Braun offers an extensive PIVC portfolio with innovative blood-control technology that helps to make the IV cannulation process cleaner, safer and more efficient.

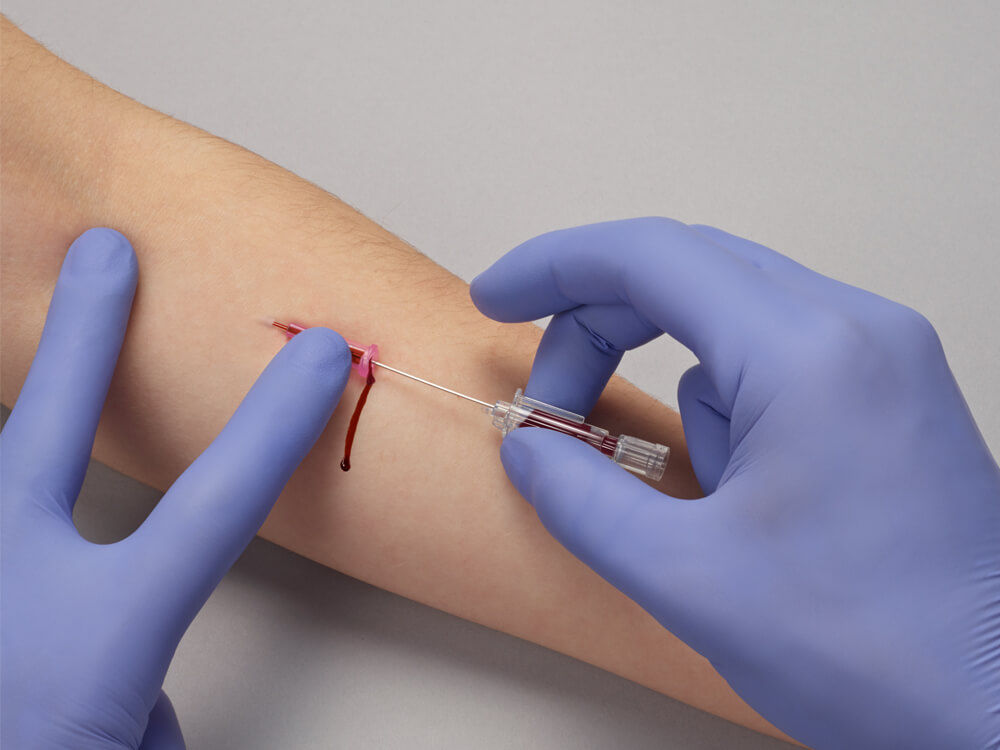
Although a routine hospital procedure, the placement of a peripheral IV catheter (PIVC) can be a complex process which may lead to complications such as blood exposure.
Blood exposure may occur during insertion, handling and disposal of an IV catheters where blood may spill on the bed, floor, clothes, gloves, unprotected skin or dressings. The resulting cleaning and disinfection work requires additional time and is associated with increased cost.1
Up to
0%
Of all healthcare workers come into involuntary contact with blood or body fluids at least once a year1
In up to
0%
Of conventional peripheral IV catheters, blood leakages occur during insertion.2
In up to
0%
Of conventional peripheral IV catheters, blood leakages occur during (dis-) connections.2
In principle, blood exposure can happen every time a catheter is placed, connected or disconnected to other Luer devices or removed.1
Main causes identified for blood exposure and spillage are blood splashes, blood back-flow from catheter hub and insufficient compression of punctured vein during connection and disconnection of Luer devices.1-4
Blood may spill onto the bed, dressings, floor, clothing, gloves, unprotected skin and dressings, causing interruptions of the tight clinical workflow.
The interruption of the tight clinical process through blood exposure and spillage is a major inconvenience for staff and patients. Clinical activities have to be stopped to change bed linen or clothing, clean and disinfect the working environment and/or exchange contaminated dressings.1
This requires additional time that is usually not available in the daily hospital routine, leading to higher stress levels and dissatisfaction for staff as well as lack of understanding among patients. In addition, more material is required for the extra cleaning efforts which can increase overall costs.
Approx.
0min
Cleaning the workplace5
Additional
0h
Time required for dressing changes per 1,000 IV catheters6, 7
Approx.
0$
Average monthly cost of cleaning and disinfecting after a blood exposure in a hospital with 4,000 IV catheters1
Preventive measures and protection of clinicians from blood exposure include
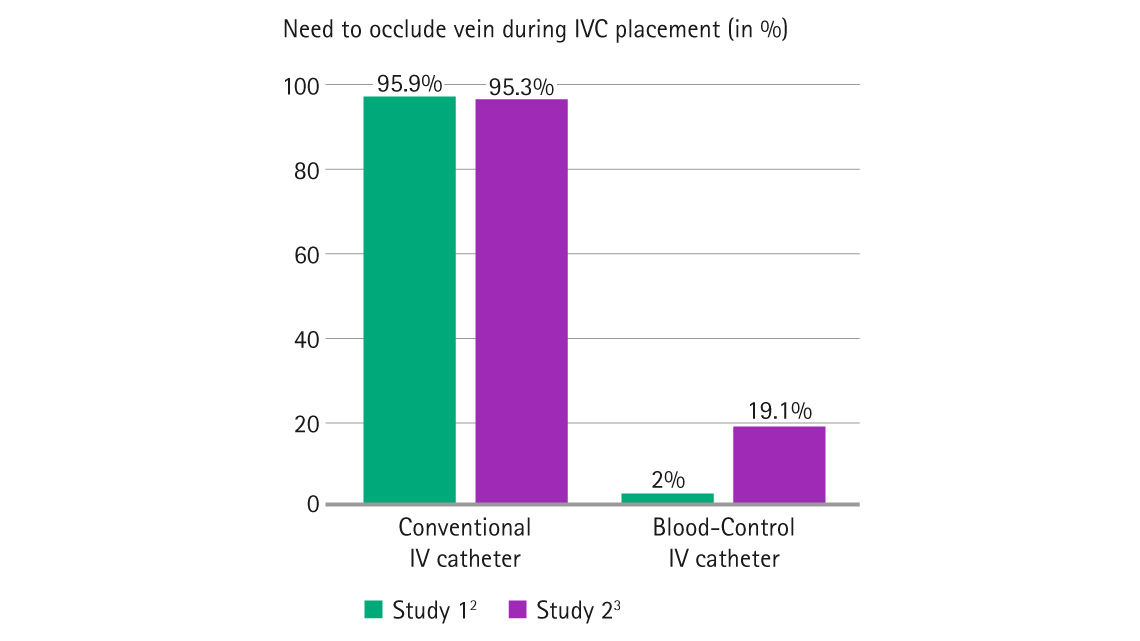
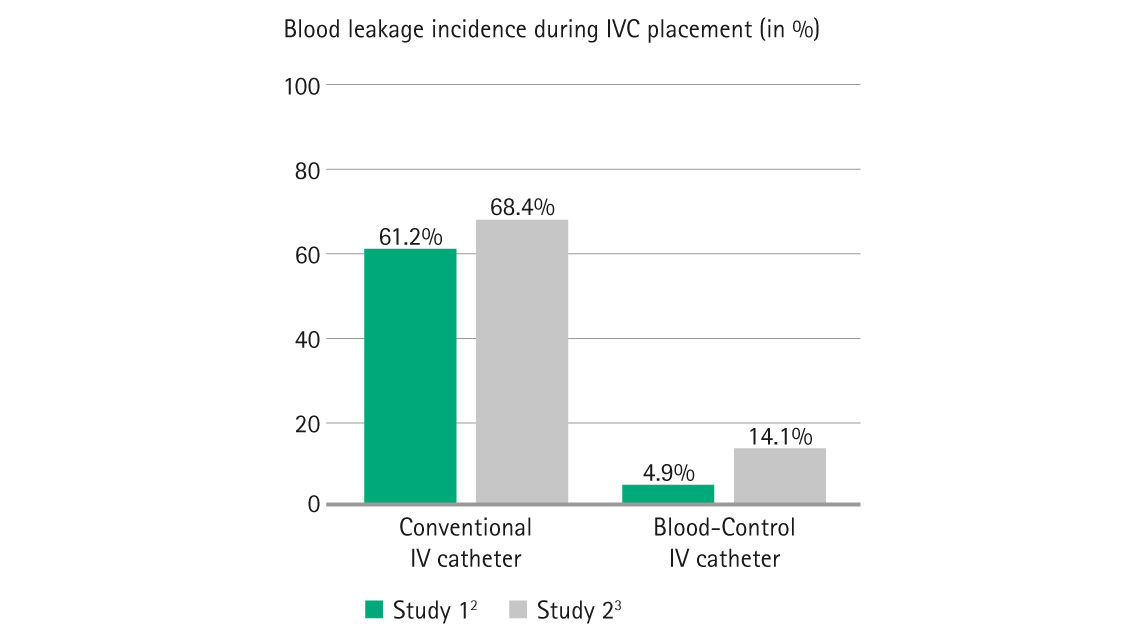
Studies have shown that the use of blood-control IV catheter can significantly reduce the risk of blood leakage and related costs (e.g. clean-up material).2,3 Due to the blood-control feature, the IV cannulation process is easier, takes less long and is more efficient as clinicians can omit occluding the vein and have their hands free to connect Luer devices.
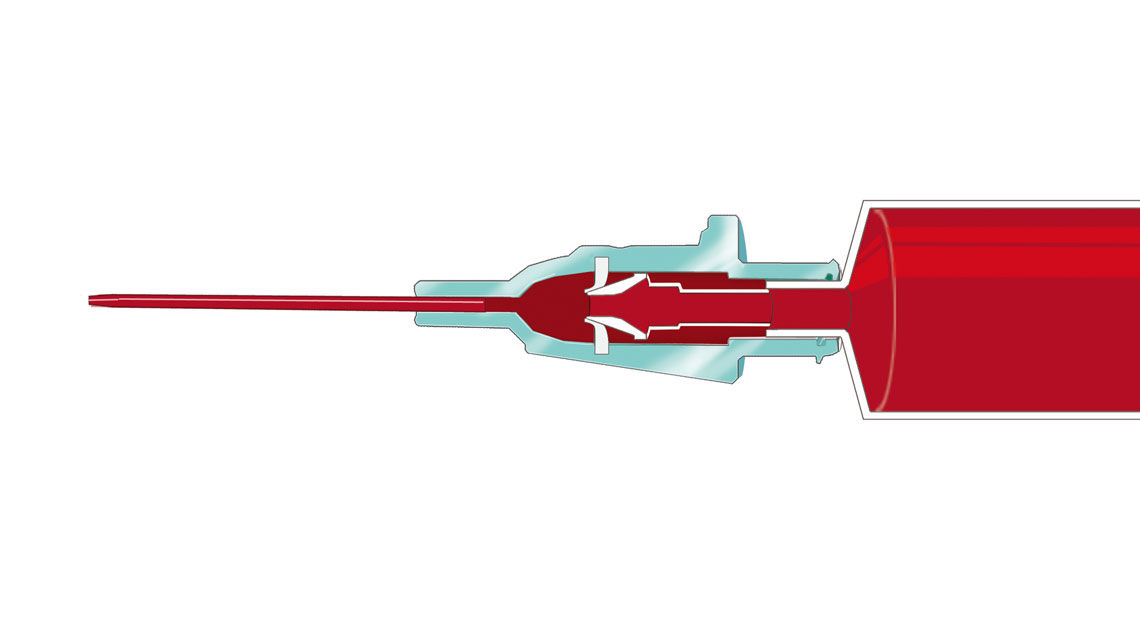
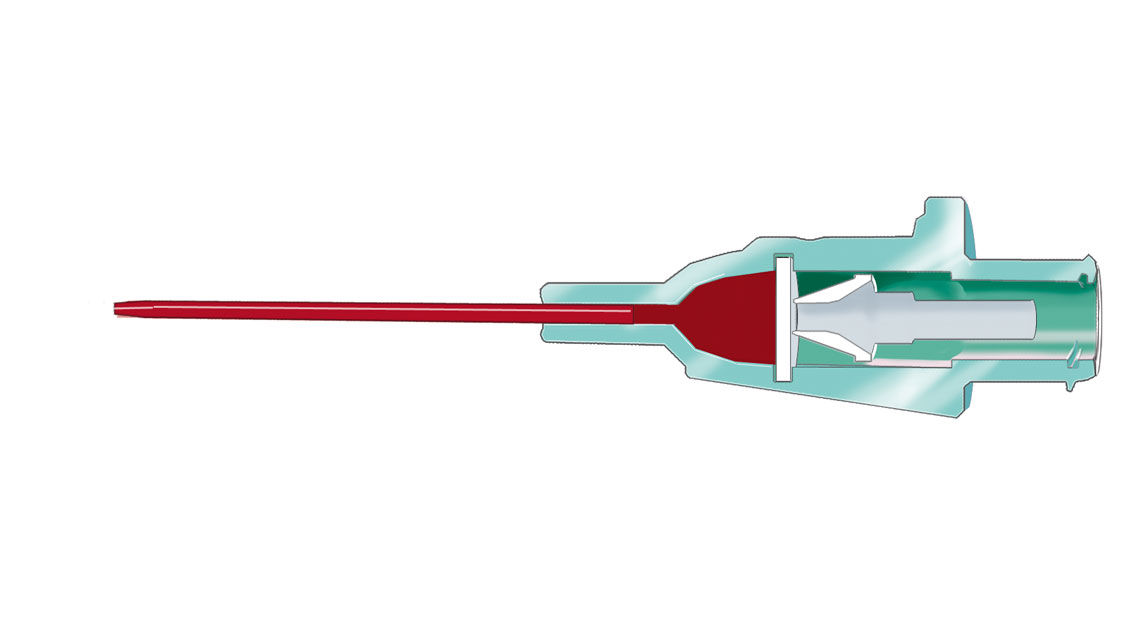
The multi-access blood control septum of Introcan Safety® 3 and Introcan Safety® 2 controls the flow of blood coming out of the catheter hub.
The blood-control feature works multiple times, thus helping to reduce blood exposure and spillage along the entire IV process.
Septum closes when the needle is removed from the catheter hub. The blood flow is controlled.
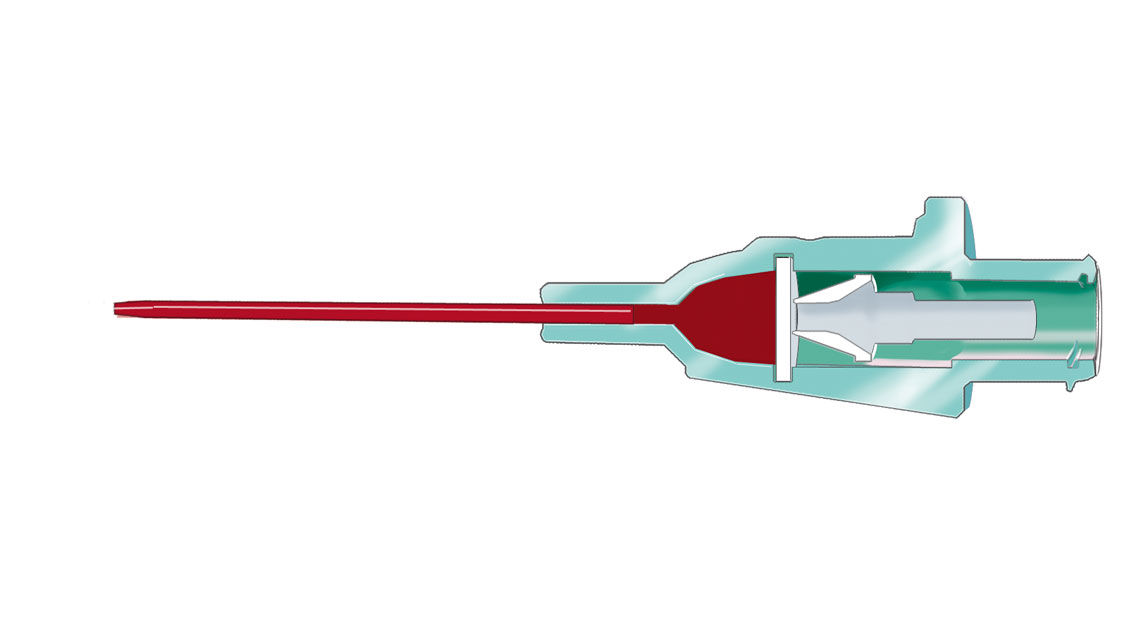
Septum closes when the needle is removed from the catheter hub. The blood flow is controlled.
Septum closes once the Luer device is removed from catheter hub. The blood glow is controlled again.
[1] Richardson D, Kaufman L. Reducing blood exposure risks and costs associated with SPIVC insertion. Nurs Manage. 2011 Dec;42(12):31-34.
[2] Haeseler G. Hildebrand M. Fritscher J. Efficacy and base of use of an intravenous catheter designed to prevent blood leakage: a prospective observational trial. 2015. J Vasc Access: 1-4.
[3] Seiberlich LE, Keay V, Kallos S, Junghans T, Lang E, McRae AD. Clinical performanceof a new blood control peripheral intravenous catheter: A prospective, randomized controlled study. Int. Emerg. Nurs. 2016 Mar
[4] Jagger J. Perry J. Parker G. Phillips EK. Nursing 2011 survey results: Blood exposure risk during peripheral I.V. catheter insertion and removal. Nursing. 2011;41(12): 45-49.
[5] Estimation based on NHS. The Revised Healthcare Cleaning Manual.
https://www.ahcp.co.uk/wp-content/uploads/NRLS-0949-Healthcare-clea-ngmanual-2009-06-v1.pdf .2009
[6] Estimation based on 1,000 conventional PIVC x 74% cases of blood exposure during (dis-) connections [2] x 1.5 min for dressing change [7].
[7] 3M UK & Ireland: 3M Tegaderm Transparent I.V. Dressing, 1633 Application and Removal [web streaming video]: Youtube; 2019 [cited 2021 Oct 25]. Available from: https://www.youtube.com/watch?v=N_y09xfFlKo