No content results match your keyword.
Content
You have successfully logged out.
Not registered yet?
No content results match your keyword.
Content
No product results match your keyword.
Products
Renal failure diagnosis
Hearing the phrase ‘you have renal failure’, can be a frightening moment. These feelings are usual. Lots of questions will come to mind – the most important of all: 'What will happen to me?'

Even though the news is life changing, there is also real cause for optimism thanks to modern medicine. This page offers answers for patients who have just been diagnosed with renal failure. Your doctor will provide support and advice with regard to the selection of the most appropriate treatment and medication in your present situation. Do not hesitate to ask, if you have any questions.

The kidneys are vital organs. They are responsible for the removal of waste products from the body, the regulation of body fluids and the production of some hormones. When kidneys can no longer perform these functions at sufficient capacity, the result is kidney disease, also called renal failure. Usually, renal failure occurs as a result of a gradual decrease in the efficiency of the kidneys over a long period (chronic kidney disease). Many conditions can lead to chronic kidney disease; the most frequent include diabetes, chronic kidney inflammation, high blood pressure and vascular damage. In some cases it is the consequence of sudden kidney failure or acute kidney injury.
Modern medicine can compensate the effects of renal failure, allowing people to live an active life despite the failure of a vital organ. However, until now there is no cure for renal failure. When a person's kidneys fail, there are three main treatment options: haemodialysis, peritoneal dialysis and kidney transplantation. No treatment modality excludes the other. Most patients who receive a transplant have experienced months, or even years, on dialysis. And although transplants can last many years, there may be a time when you will need dialysis again in the future. Your doctor and nursing staff will support you through all stages of your kidney disease and all conditions of your life. So do not hesitate to ask, even if you think your question might not be directly related to your treatment.
Haemodialysis is the most common method used to treat end stage renal disease (ESRD). The process of haemodialysis cleans your blood using a special type of filter called a dialyzer. It is mostly performed at a renal care centre under the supervision of experienced and well-trained medical staff.
Learn more about haemodialysis
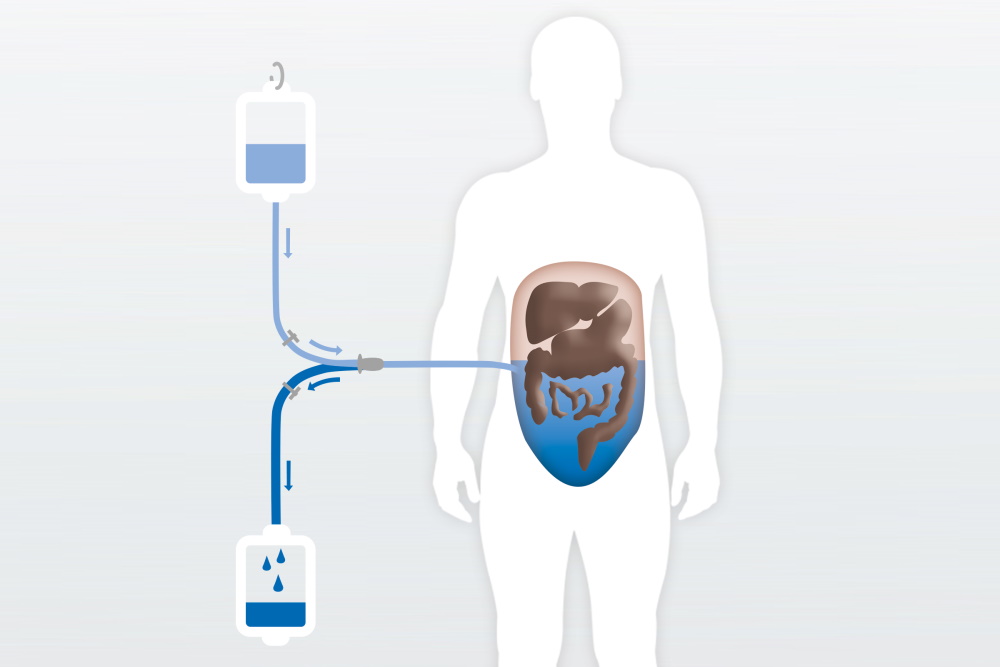
In this form of therapy, the cleaning function of the kidneys is supported or carried out by the peritoneum of the abdominal cavity. A minor surgical procedure is used to permanently insert a soft tube or catheter into the abdominal cavity.
This cycle is usually repeated about four times a day but can also be performed once per day under special circumstances. It must be performed carefully to avoid risks like peritonitis which is an infection of the peritoneum. This procedure is easy to learn. That is why patients can carry out this form of dialysis treatment unassisted and in the comfort of their own homes.
The solution for peritoneal dialysis is a sterile fluid mainly consisting of glucose or amino acids which helps with waste removal by the peritoneum.
/
The solution flows into the catheter inserted by a minor surgical procedure into the abdominal cavity.
/
In this form of therapy, the cleaning function of the kidneys is supported or carried out by the peritoneum of the abdominal cavity. The solution binds waste products, which are filtered through the peritoneum.
/
After several hours, the dialysis solution is saturated with waste products from the blood and is drained from the abdomen, then replaced by fresh solution in order to continue the cleaning.
/
Once saturated with waste products from the blood the dialysis solution is drained from the abdomen into a drainage bag.
/
A kidney transplant is often a long-standing wish of many kidney patients. For many, it means returning to a life without being dependent on renal care centres, a restrictive time schedule and diets, being able to work without constraints and the option to travel more easily. This desire takes concrete form when an appropriate donor kidney is found.

Many patients feel that their quality of life improves after a transplant, compared to being on dialysis. It can offer more freedom because you no longer need to attend for dialysis, and there is no real diet or fluid restriction.
However, if you are waiting for a cadaveric kidney, it may take months or even several years until an appropriate donor kidney is found. It is difficult to say how long you may have to wait, some people are fortunate and receive a transplant quickly, others will spend longer on the waiting list. This waiting time can be difficult for some patients to cope with, and can cause frustration and stress. These feelings are natural, and your doctor and nursing staff will help you to cope with any concerns you may have.
Kidney transplantation requires an operation to transplant a healthy kidney from another person into your body. Various tests have to be completed before an operation date can be scheduled. During the operation the kidney is placed into your lower abdomen and is joined to your artery and vein. The blood then passes through the transplant and it starts to make urine.
It is also important to know that the kidney transplantation does not heal the kidney disease. To protect your kidney from rejection by your body or recurrence of the underlying kidney disease, daily medication and regular consultations with your doctor are vital.
Please always consult your nephrologist.
Find out how the almost 70-year-old success story of kidney transplants offers more options than you might think.
Go to the special topic article on page 6 of our Share for Care magazineAs a haemodialysis or peritoneal dialysis patient, you will have different medications prescribed for different purposes. You should always be aware of all medication you take, meaning that you should know their names, purpose and how they are administered. Whenever you have problems with your medications or any questions, do not hesitate to contact your doctor or nursing staff in your renal care centre. Impaired renal function and haemodialysis can drastically alter the effects of medication. Consult your doctor before making any changes to your current medication. The following medications are used most frequently:
Many patients suffer from high blood pressure (hypertension). Hypertension can harm you. Therefore, blood pressure has to be regulated with appropriate medication and carefully monitored especially during treatment.
Erythropoietin, often referred to as EPO, is a hormone produced by the kidneys that stimulates the bone marrow to produce red blood cells. Since the production of erythropoietin in chronic kidney disease patients is reduced, the number of red blood cells is also reduced. This is the main aspect leading to a condition known as renal anemia. Synthetic erythropoietin can be given intravenously or through the skin as a substitute for natural erythropoietin in order to maintain an adequate number of red blood cells. It may also be given through the bloodlines of the dialysis machine during the dialysis treatment.
Iron is a vital building block of haemoglobin, the key protein found in normal red blood cells. Without iron, it is difficult for the body to create enough healthy red blood cells. This is why iron supplementation is mostly necessary in addition to EPO. Iron is usually supplied by an intravenous infusion at the renal care centre.
Our kidneys normally excrete the phosphate that is absorbed with food. In chronic renal failure, this no longer happens. Therefore, phosphate levels in the body increase and, in combination with other substances, cause irritation to blood vessels, bone and sometimes the skin. A major side effect of increased phosphate levels can be arteriosclerosis, i.e. calcification of the blood vessels, which can lead to heart disease. Dialysis helps in this regard, but it can only eliminate some of the excess phosphate. This means that phosphate levels in the body must be lowered further by means of a low phosphate intake and appropriate medications, known as phosphate binders. These medications ‘bind’ the phosphate in the gut so that it cannot be absorbed into the bloodstream.
Vitamin D is activated in the kidneys and is needed for multiple functions in the body. For example, it is needed for healthy bones. People with kidney disease are often prescribed vitamin D in a pre-activated form as their kidneys cannot activate the vitamin D anymore.
You need dialysis because you have suffered renal failure. Your kidneys have stopped – or almost stopped working. The kidneys are the body’s filter system for getting rid of toxins and chemicals that the body does not need and that might harm you. Renal failure, if left untreated, is fatal, but modern medicine has provided us with life-sustaining treatments, including haemodialysis.
Haemodialysis and peritoneal dialysis have been done since the mid-1940s. Dialysis was established as a regular treatment in 1960 and is now a standard treatment all around the world. Continuous ambulatory peritoneal dialysis (CAPD) began in 1976. Thousands of patients have been helped by these treatments. Dialysis is now a well-established procedure, with thousands of patients receiving treatment around the world.
No. Dialysis treatment only replaces several kidney functions.That’s why it is commonly called renal replacement therapy. However, there are currently a lot of different treatments for kidney failure and more and more treatments are under investigation. In general, these treatments only help to slow down progressive kidney function loss and cannot completely stop this loss or reverse it. That’s why we need kidney replacement therapies like haemodialysis or kidney transplantation.
Renal failure is uncomfortable, life-threatening and accompanied by various severe symptoms. Dialysis therapy helps significantly to improve all of these disadvantages, but it cannot cure the renal failure. Frequent communication with your medical support staff in an open atmosphere will help you to get the most appropriate and convenient therapy.
We cannot promise that you will feel as well on dialysis as you did before renal failure, as there is no real substitute for your own healthy kidneys. But to keep you as well as possible your treatment will consist of three main elements: dialysis, diet and drugs. The haemodialysis diet is quite strict and can take some time getting used to. There will be limits on your intake of fluid, and you will need to be careful of foods high in sodium and potassium. But with imagination you can still cook tasty meals. Your care team will also explain your diet to you in detail. There are a number of drugs which you need to take to help prevent some of the complications of dialysis. However, there will be times when you will feel tired and fed-up. This is the same as with any chronic condition. But with care and by following the advice you are given, you will be able to carry out most normal activities.