No content results match your keyword.
Content
You have successfully logged out.
Not registered yet?
No content results match your keyword.
Content
No product results match your keyword.
Products
Haemodialysis
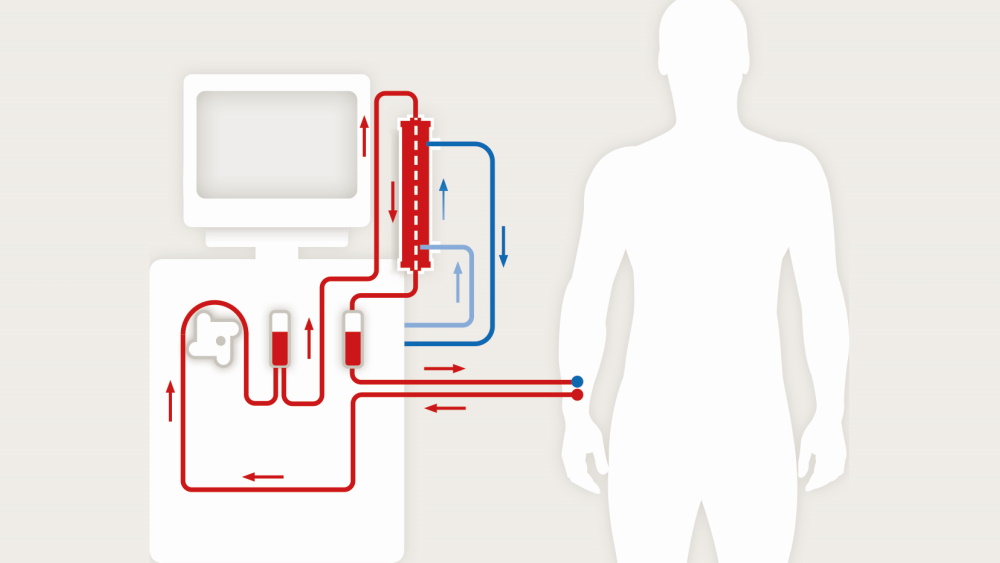
The process of haemodialysis cleans your blood using a special type of filter called a dialyzer. To perform this dialysis therapy, relatively large quantities of blood must be handled in a relatively short period of time.
Haemodialysis is the most common renal replacement therapy used to treat chronic kidney disease. It is mostly performed at a renal care centre under the supervision of experienced and well-trained medical staff. During treatment, the blood is cleaned in the dialyzer. The cleaning process normally shouldn't cause any pain and many patients will experience improvement of their condition especially in the beginning of dialysis treatment. However, if you feel unwell or uncomfortable during treatment, you should tell the staff, who will help you. Depending on your medical history, you will usually undergo haemodialysis three times a week with an average session time of 4-5 hours each treatment.
A special vascular access point is established to support chronic dialysis treatment – a so-called AV (arteriovenous) fistula or shunt. Alternatively, a central venous catheter (CVC) can be used.
/
During hemodialysis therapy the blood is removed from your body to be detoxicated.
/
A pump on the dialysis machine pumps the blood from your body through the dialyzer and back to you.
/
Dialysate is a solution of pure water, electrolytes and salts, such as bicarbonate and sodium. The dialysate circuit is separated from the part of the blood circuit by the dialyzer membrane.
/
For haemodialysis, good vascular access is critical to being able to carry out dialysis treatment. It involves the use of blood vessels, which are often not easily accessible or have too little pressure. Therefore, many patients have a vascular connection, also known as AV fistula or dialysis shunt. This is the most common method used for vascular access.
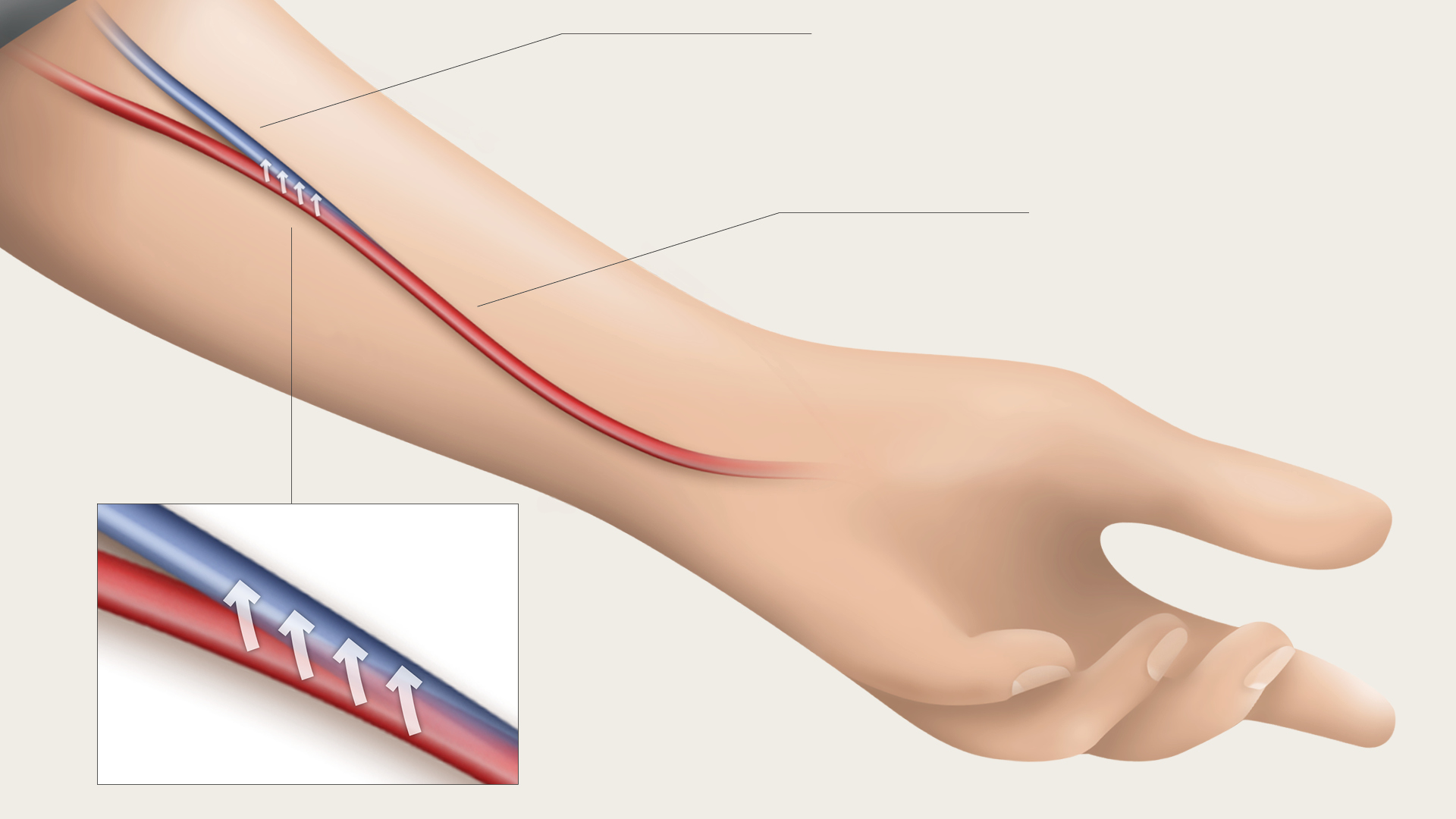
For hemodialysis, good vascular access is critical to being able to carry out dialysis treatment. Therefore, many patients have a AV fistula, placed between the artery and vein of the forearm by means of a surgical procedure.
/
Creating a fistula involves a small intervention on the wrist or arm to join together a vein and an artery. The operation takes about an hour. It is usually carried out under local anaesthetic and you will spend part of the day in hospital. Joining a vein to an artery creates a pulsatile, a faster and more turbulent flow of blood through the vein. This makes the vein wall thicker and it gets bigger. Eventually, it becomes visible under the skin, looking a bit like a large varicose vein. When you touch it you can feel a “buzz”. This sensation is very important, because it means that the fistula is working properly.
The fistula heals within a few days, but it requires several weeks before it is ready for full use as a vascular access point. Watch carefully for signs of infection: redness, swelling, pain, high pulse rate and fever. If you notice any of these signs, contact your renal care centre immediately.
In addition to the AV fistula, there are two other main types of vascular access for haemodialysis treatment: the vascular access graft as well as the central venous catheter.
A graft is a small piece of plastic inserted between an artery and a vein in the arm or thigh. If a patient’s veins are too small or weak for an AV fistula to be created, a synthetic graft (made from synthetic material) or a natural vein, e.g. from your calves, may be used to form a connection between an artery and a vein. It is placed under the skin like a natural vein. Compared with arteriovenous fistulas (AVF), the grafts (AVG) tend to have more problems with clotting or infection and need to be replaced sooner,but if well-managed a graft can last for years. The graft, as well as the AV fistula, lie beneath the surface of the skin.
A catheter may be used when, for some reason, a fistula is not possible or if an AV fistula is not ready when starting dialysis. A central venous catheter is a plastic tube placed into a central vein in the neck or chest by a doctor. Temporary catheters are held in place with stitches. Permanent catheters, intended for long-term use, may be held in place by a special cuff under the skin and a few stitches. About six inches of the tube protrude from your skin and a dressing is placed over the site where it enters your skin. The dressing should be kept clean and dry and extra care is needed when bathing and washing your hair. The tube is easily covered by clothing.
Catheters can clog, become infected, or cause narrowing of the veins in which they are placed. With good care, a catheter can be a helpful ‘bridge’ while your fistula or graft is healing or can allow you to have dialysis when other forms of vascular access are not available.
As catheters are prone to infections, it is highly recommended that the following principles are considered:
In principle, patients with end stage renal disease suffer from the toxic effects of waste material produced by their own metabolism. Healthy kidneys serve as the purification plant of the body and this function is missing when the damaged kidneys can no longer adequately purify the blood. During haemodialysis therapy the blood is removed from your body, detoxicated and then returned to your body. That is why dialysis is often called an “extracorporeal treatment” – as the purification function of the kidneys has now been transferred to a machine outside the body. With today’s modern medical possibilities, there are multiple ways of providing extracorporeal detoxification. Your medical doctor will inform you which modality and treatment settings are most appropriate for you.
As we have already seen the dialyser has two main parts: one part for your blood and the other for the dialysate. Both of these parts are separated from each other by the dialyzer membrane. The blood and dialysate are never mixed and kept separate at all times. Blood cells, proteins and other important things remain in your blood because they are too big to pass through the membrane. Smaller waste products such as urea, sodium and potassium as well as excess fluid pass through the membrane and are removed. Changes in the dialysate fluid can be made to suit your specific needs and are determined by your dialysis prescription.
Mostly waste products of the corporeal metabolism are removed. Because each individual’s nutrition is different, there are different amounts of metabolism end products that need to be removed for each person. Healthy kidneys also regulate the composition of special components like electrolytes, water, minerals, trace elements, etc. It is therefore necessary for the dialysis machine to also take over these regulating tasks in addition to removing toxins. This plays a role, for example, in patients with acid-base disturbances, which is very common in dialysis patients.
The efficiency of dialysis is dependent upon the ability to get blood from you and to pass it through the dialyzer. This is achieved by using the vascular access that you currently have. Blood tubing is attached to your access and a pump on the dialysis machine pumps the blood from your body through the dialyser and back to you. You will notice that the blood runs in a continuous circuit: from you to the dialyzer and then back to you. This means that only a small amount of your blood is outside of you at any one time.
The haemodialysis machine has a number of different functions, all designed to make your treatment as efficient and safe as possible. It is like a large computer and a pump. As well as pumping blood from you to the dialyzer it keeps track of:
It is also responsible for mixing the dialysate concentrate and the pure water. This is responsible for helping to pull out the toxins across the dialyzer membrane.
Once you have been “connected“ and the dialysis treatment has started you are free to do what you wish – as long as you remember that you are restricted to the dialysis chair. There are many things you can do during your treatment:
The nurse will also check your blood pressure and pulse at least once every hour, and will make a note of the machine settings to ensure your treatment is progressing correctly. There will also be time for you to ask questions about dialysis.
One of the functions of the dialysis machine is to monitor your treatment intended to ensure that you are safe during your dialysis treatment. Throughout dialysis it measures pressures inside the blood tubing and dialyzer. The dialysis machine also measures the blood flow, temperature and the correct mixing of the dialysate. When your treatment starts your nurse will set limits to all these pressures. If the machine measures any pressures outside of these limits the machine alarms to let the nurse know of the problem. With some of the alarms the machine will also stop the blood pump or dialysate flow intended to make sure that you are safe until the problem has been resolved. Then when it is time to go home it also alarms.
Cramps usually occur in the legs and can be uncomfortable. There are a number of reasons why cramps occur, and are different from patient to patient. The most common cause is linked to the removal of large volumes of fluid during dialysis. Make sure you tell the staff as soon as you feel the cramp starting so that they can help you and prevent it from getting worse.
Infection remains at risk during dialysis because of the nature of the treatment. The dialysis staff are trained in methods to reduce infection risks, but you also have a role to play. When you enter and leave the dialysis treatment room, make sure that you wash your hands. Always tell the nursing staff before you start dialysis if you believe you have some form of infection.
At the renal care centre
At home
Once your dialysis treatment has finished your purified blood will be completely returned to your body, and then you will be disconnected from the dialysis machine. If you are using a central venous catheter, this will be capped off until your next treatment. However, if you are using a fistula or graft, the needles will be removed and only when the nurse is sure that the bleeding has stopped will you be able to leave the dialysis centre. Your blood pressure will be checked to make sure it is safe for you to get off the chair. This is important as you can sometimes feel faint right after you stand up following treatment. Your weight will be checked again and recorded. This assessment is important and your nurse wants to make sure it is safe for you to leave the dialysis room and wait for your transport home. If at anytime you feel unwell, make sure you tell the nurse before you leave the renal care centre.
The specific arrangements between you and your doctor is very important here. The time needed for your dialysis depends on:
If you have had a new AV fistula created, you may be asked to carry out some exercises to help the AV fistula develop and mature. This ‘maturation process’ takes about 6-8 weeks. Small softballs developed especially for AV fistula training are best suited for this. You take the balls in your hand and squeeze them in a pumping motion. You also learn to pay attention to the thrill of the AV fistula each day. The thrill is a sign of the blood flow in the AV fistula. You can feel the thrill with your hand. Some patients also use a stethoscope to listen to the so-called murmur. Wound care and changing dressings regularly are essential when managing an AV fistula. The AV fistula arm can be cleaned by washing, typically after 12-24 hours. In the context of general personal hygiene, you may also apply cream to it using ointment that is easily absorbable. For the prevention of possible complications (such as AV fistula infections), intact skin with good protection is very important.
Since an AV fistula puncture is an invasive procedure, all the usual pre-operative hygiene measures are adhered to. This is something that dialysis staff (physicians or nurses) are fully trained for and pay close attention to. Dialysis patients should also take care of their hygiene, because they may be especially vulnerable to infections due to their disease and reduced resistance. First the AV fistula arm is washed and then cleaned using a disinfectant. The dialysis staff will use gloves and complete the process using strict infection control practices. Here, the standardised hygiene rules are adhered to by the dialysis staff.
Once the fistula has developed, it can last a very long time. Some patients have a fistula that is still working after 30 years. However, if you are elderly when your fistula is created or if you suffer from other medical conditions such as diabetes, the fistula may not last that long.
During dialysis, two needles are placed into the fistula. One needle will remove the blood and pass it to the machine so it can be cleaned. The other needle will return the processed blood to the body. The needles are attached by plastic tubing to a special filter called dialyzer. A pump pushes the blood through the dialyzer. Blood passes on one side of the filter, and solution made by the dialysis machine passes on the other side. The blood does not mix with the solution. Instead, the solution pulls extra fluid and waste out of the blood by a process called dialysis. The "clean" blood returns through the plastic tube. It passes back into the patient's body through the second needle.
Keep your fistula arm clean and wash it every day. Your nurse will be able to give you advice on the best type of cleaning material, skin care and cleansing to use. Watch for signs of infection. These may be tenderness, swelling or redness over the fistula. You may also have a fever. If you think the fistula has stopped working or that you have an infection, immediately contact the dialysis centre for advice. Avoid wearing tight clothing or a wristwatch on the access arm. Avoid having your blood pressure taken on the arm with the fistula. Avoid having blood samples taken from the arm with the fistula (except during HD treatment or with the renal unit's approval). Avoid sleeping on the fistula arm. Avoid carrying heavy shopping bags on the fistula arm.
Always wash your access arm before each dialysis treatment. Don’t touch the skin around your access after the nurse has cleaned your arm in preparation for inserting your needles. Don’t cough or sneeze on the access site during dialysis. When your needles have been removed, apply only gentle pressure to stop bleeding. And press only where the needle has been. When you get home, don’t scratch around the needles sites and don’t pick off any scabs.
If you check your fistula and think you cannot hear or feel the blood going through the fistula, it may have clotted or stopped working. Phone the dialysis centre immediately for advice. It may be possible to “rescue” the fistula. Do not wait until your next scheduled dialysis day, it is important to notify your centre immediately.